Conventional therapy
Surgery is the mainstay of treatment for localized melanoma [1, 2]. Radiotherapy [3] and systemic chemotherapy [1, 2, 4] have a limited (if any) survival impact on the control of metastatic disease, due the resistance of melanoma cells to the cytotoxic effects of these conventional antineoplastic agents at the maximum tolerable doses. To some extent, biotherapy (i.e. interferon-alpha, IFN) appears to improve patients survival under certain clinical circumstances [1, 2, 5, 6].
Primary tumor
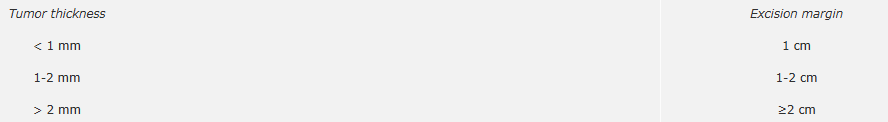
Radical (margin-free) excision is the treatment of choice for primary melanoma. According to the results of five randomized controlled trials (RCT) [7-11], the currently recommended excision margins are the following [1, 2]:
Importantly, the above mentioned RCT demonstrated that the width of the excision margin only influences the local recurrence rate or disease-free survival, but not overall survival.
Regional lymph nodes
Phase III RCT have demonstrated that elective radical lymph node dissection (RLND) - i.e. prophylactic lymphadenectomy in the absence of clinical evidence of metastatic disease - does not provide any significant survival advantage over therapeutic lymphadenectomy (i.e. lymph node dissection performed once metastatic lymph node disease becomes clinically evident) [12, 13].
RLND of the regional basin(s) in patients with clinical evidence of lymph node metastatic disease is considered the current standard of care [1, 2]. In fact, although no RCT has demonstrated a survival advantage, a significant number of patients attain 5-year survival. Furthermore, the palliative benefits of RLND are considerable, as untreated lymph node metastatic disease can be expected to ulcerate, impinge on neural structures, and cause pain in patients whose life expectancy is longer than one year.
The clinical implementation of both sentinel node biopsy (SNB) and interferon-alpha (IFNα) based adjuvant therapy has re-opened the debate: in fact, it is not clear whether the early detection of lymph node metastasis might affect patients' survival directly and/or through the early submission of patients to a potentially effective adjuvant treatment (see Sentinel lymph node section). At the time of writing (May 2007) only the results of one such RCT are available and do not support a therapeutic effect of SNB, at least with the current eligibility criteria [14].
Adjuvant therapy
The poor prognosis of melanoma once it has metastasized to the regional nodes or beyond and its relative resistance to available chemotherapeutic agents have prompted the search for an effective therapy in the adjuvant setting through a variety of different approaches [5, 15].
Tens of RCT involving a host of different agents showed no convincing evidence of a survival advantage with the use of adjuvant therapy [5, 15]. Of note, many of these trials were small studies employing heterogeneous groups of patients with varying risks of recurrence and thus were underpowered to detect significant results.
More recently, favorable results [16] observed with high-dose IFNα prompted the approval of this cytokine for the adjuvant treatment of high risk (TNM stage III) melanoma patients. However, other phase III RCT yielded conflicting results [17-20]. Reviews (including a meta-analysis) of available data indicate an improvement in disease-free but not overall survival [5, 6].
In-transit metastasis
Few and small in-transit metastases can be best managed by surgical excision. However, when multiple bulky nodules occur, their treatment can be highly challenging.
If confined to an extremity, in-transit metastases can be treated with isolated limb perfusion (ILP), a surgically demanding locoregional treatment that delivers high dose of antineoplastic drugs (usually melphalan, tumor necrosis factor alpha, TNF) into the affected limb with minimal systemic toxicity [21, 22]. Although this locoregional treatment achieves high response rates (up to 90%), no survival benefit has ever been demonstrated [23].
Distant metastatic disease
The treatment of metastatic melanoma is currently a frustrating challenge for clinicians due to the very poor results obtained with available therapeutic modalities [1, 2], which urges investigators to make any effort to develop novel anti-melanoma strategies (see Molecularly targeted therapy section) and to enroll patients in clinical trials testing new therapeutic regimens.
When single metastatic lesions are detected (mainly in lungs, soft tissues, brain and intestine), surgical metastasectomy is often performed, and retrospective reviews have reported a survival advantage in selected operated melanoma patients compared with historic controls [24]. However, the efficacy of surgery remains controversial because of the likelihood of widespread disease at other sites; moreover, no RCT exists to support this therapeutic option.
Radiotherapy is mainly proposed for symptom palliation in case of localized (usually unresectable) metastatic disease [3, 25]. Relief of symptoms can be temporarily achieved by radiation therapy in patients with metastatic disease to the bone or the brain.
Despite its unproven efficacy, systemic chemotherapy remains the most widely used treatment for patients with metastatic melanoma, especially in case of unresectable metastatic disease [1, 2, 4, 26]. Chemotherapeutic agents that have been most widely applied in metastatic disease are dacarbazine (DTIC), the platinum analogs, nitrosoureas, and microtubules toxins.
DTIC is considered the reference agent for melanoma, with an overall (complete + partial) response rate ranging from 14% to 20% (complete response rate < 5%) and a median response duration ranging from four to six months. Long-term follow-up of patients treated with DTIC alone indicates that less than 2% of patients survive 6 years, and RCT have shown no survival advantage over best supportive care.
Temozolomide is a non-classical prodrug of MTIC (5-(3-N-methyltriazen-l-yl)-imidazole-4-carboxamide), the alkylating agent that is the active metabolite of DTIC. Temozolomide spontaneously converts into its active metabolite and in several trials has shown antitumor activity against melanoma that is at least equivalent to that of DTIC. The most attractive advantage of temozolomide is the well-documented penetration of third spaces such as the central nervous system and the ascites fluid. A RCT comparing temozolomide with DTIC failed to demonstrate improvements in survival, which has tempered the initial enthusiasm for this antineoplastic agent.
Given the failure of single agent regimens, polychemotherapy has been tested for the treatment of melanoma. DTIC-based combination regimens (e.g. DTIC + cisplatin + vinblastine, DTIC + cisplatin + carmustine + tamoxifen, DTIC + taxanes + temozolomide + cisplatin) have been associated with higher tumor response rates (up to 40%), but no survival advantage over DTIC alone has ever been demonstrated. Biochemotherapy often results in higher responses, but its impact on overall survival has been disappointing (according to the results of RCT) and its toxicity is remarkable [27]. Overall, to date RCT have shown no compelling evidence to support the value of combination systemic chemotherapy.