Dermoscopy
The ABCDE rule (asymmetry, irregular borders, multiple colors, diameter >6 mm, enlarging lesion) contains the main clinical criteria for naked-eye based diagnosis of suspected cutaneous malignant melanoma (CMM). The early phase of malignant melanoma is difficult to identify because CMM can share many clinical features with an atypical nevus. In fact several studies have described diagnostic accuracy rates ranging from 50-75% [1,2], indicating a need for additional diagnostic tools, in particular to detect the so-called small melanomas as well as melanoma regular in shape or color [3-5].
Over the last 20 years, dermoscopy (i.e. dermatoscopy, epiluminescence microscopy [ELM], surface microscopy) has opened a new dimension in the examination of pigmented skin lesions (PSL) and, especially, in the identification of the early phase of CMM [3-33].
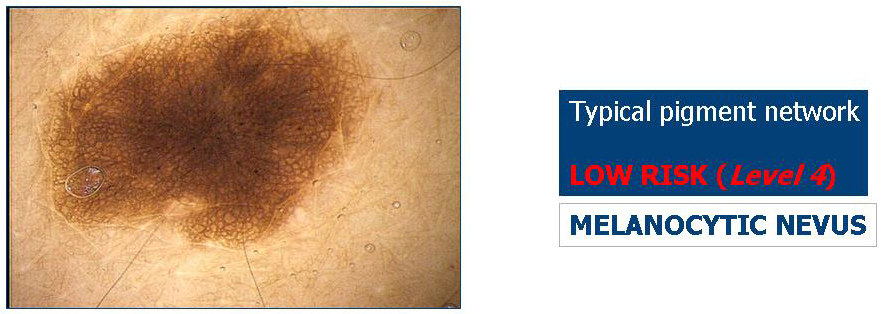
Dermoscopy is a non-invasive method that allows the in vivo evaluation of colors and microstructures of the epidermis, the dermo-epidermal junction, and the papillary dermis not visible to the naked eye (FIGURE 1). These structures are specifically correlated to histological features [5,6].
Based on the results of meta-analyses, dermoscopy is more accurate than clinical examination in the diagnosis of pigmented skin lesions [8,9]. However this technique must be considered as a valid support, but not a substitute, in the clinical diagnosis of melanoma [5,29-32].
FIGURE 1: Clinical (upper panel) and corresponding dermoscopic image (lower panel) of a melanocytic nevus. Dermoscopy shows symmetry in pigmentation and structures throughout the lesion with globules symmetrically distributed at periphery.
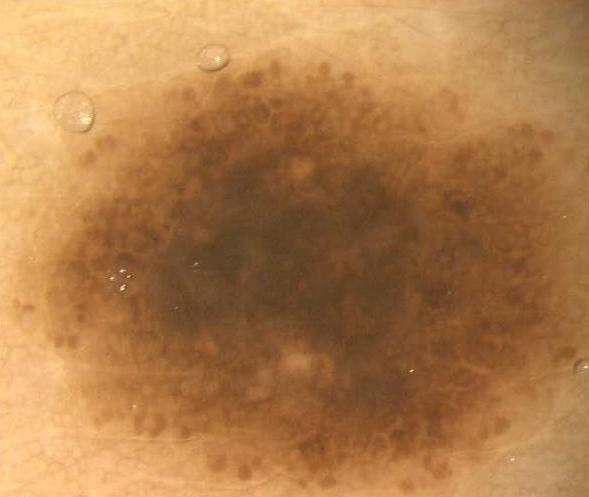

Dermoscopy involves the evaluation of the skin surface. During a dermoscopy assessment, the PSL is covered with a liquid (usually oil or alcohol) and examined under a specific optical system. Applying oil reduces the reflectivity of the skin and enhances the transparency of the stratum corneum. This allows visualization of specific structures related to the epidermis, the dermo-epidermal junction and the papillary dermis, and it also suggests the location and distribution of melanin (FIGURE 1).
Numerous instruments (FIGURE 2) are utilized for dermoscopic examination, such as conventional contact dermoscope, contact polarized light dermoscope, non-contact polarized light dermoscope, stereomicroscope, videodermoscope, digital camera. These instruments and the corresponding techniques can be equivalent and/or complementary and can influence the inter- and intra-observer reproducibility [10-15].
FIGURE 2: Dermoscopy instruments (in order of appearance, from top to bottom): dermatoscope; hand held stereomicroscope; stereomicroscope; digital epiluminescence by stereomicroscope; videomicroscope; digital camera.



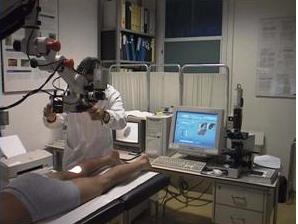


The dermatoscope is the standard piece of equipment used to perform a dermoscopy examination (FIGURE 2). It is similar to an otoscope, is user friendly, and is inexpensive. These optical system's features include monocular observation, 10x magnification, and the use of an illumination system (3.5-V halogen lamp).
Recently the use of dermoscope with light-emitting diode (LED) lighting and polarizing filters for glare reduction eliminates the need for skin contact and the required liquids. Although these latter instruments are very useful for rapidly screening pigmented lesions in patients with multiple nevi, the clinical images can be different from those attained using conventional glass plate liquid-surface microscopes. For these reasons it has been suggested to use cross-polarized surface to rapid screening of pigmented lesions, with a final definitive diagnosis dependent on glass plate liquid instruments.
Furthermore digital epiluminescence microscopy system combined with a digital camera can capture a high quality, glare-free image (FIGURE 2).
Documenting lesions is simple for training, teledermoscopy, pre-surgical evaluation and mole mapping.
Another optical instrument, the stereomicroscope, allows for an accurate binocular observation with different magnifications (6x-80x) (FIGURE 2).
The illumination system includes a halogen lamp (12 V/50 W).
From an empiric point of view, visualization is better than with the dermatoscope, but formal studies of the differences in diagnostic features and accuracy of the two instruments have never been published.
Features of another optical system, the videodermatoscope, include a video probe that transmits images of the PSL to a color monitor (FIGURE 2).
The addition of a digital system to the stereomicroscope (also termed the digital epiluminescence microscope) or to the videodermatoscope has opened a new area in the field of skin cancer diagnosis with the advantages of computerized technology.
However, the technologic features (which are cost dependent) of the camera (single-chip video charge-coupled device, 3-chip charge-coupled device, or still digital), optical system, monitor, digitized board, and software significantly influence the resolution and quality of the images.
Accurate evaluation of the PSL color, degree of pigmentation and distribution of the colors within the lesion are the most important elements of a dermoscopy examination.
The epidermis usually appears white, but acanthosis results in a grayish-brown or brownish-yellow color.
Melanin is the most important pigment in determining different structural and chromatic patterns. The PSL can have a different degree and distribution of pigmentation depending on the location of melanin in different layers of the skin.
Melanin location determines the color of the lesion according to the following schema (FIGURE 3):
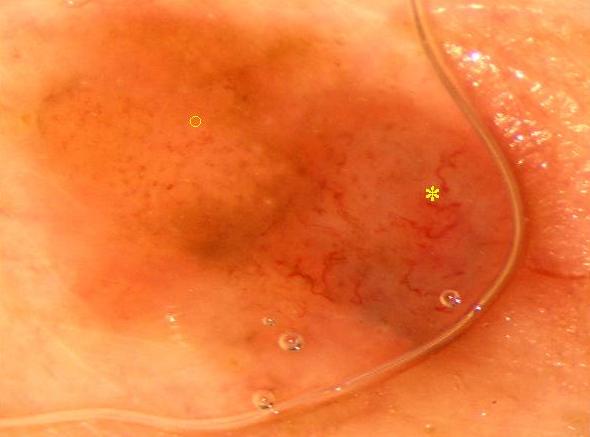
Other possible colors include various shades of white and red (FIGURE 4). White shades are related to regression and may be seen with melanomas, benign melanocytic nevi (halo nevus), and non-melanocytic lesions (lichenoid keratosis, scars). Red shades are related to increased angiogenesis in tumors, an increased number of capillary vessels, and bleeding within the lesion. If bleeding persists and crust develops, the color ranges from red-black to blue-black.
A good evaluation of colors and their relative distribution is essential for achieving the correct clinical diagnosis of a PSL.
FIGURE 3: Pigmented skin lesion (PSL) colors (in order of appearance, from top to bottom): black nevus (intraepidermal location); light-brown nevus (dermo-epidermal junction); dark-brown nevus (dermo-epidemal junction); blue nevus (dermis).








The most important epiluminescence microscopy (ELM) feature of melanocytic lesions is the pigment network (PN), which consists of pigmented network lines and hypopigmented holes.
This feature is correlated histologically to the length of the "rete ridges" and to the distribution of melanin within the keratinocytes of the epidermal "rete ridges". The network of hypopigmented holes corresponds to the suprapapillary plate, which is relatively thin and contains less melanin. The network lines correspond to the "rete ridges", which are thicker and have a greater quantity of melanin.
In normal melanocytic nevi, the PN is slightly pigmented. Light-brown network lines are thin and fade gradually at the periphery. Holes are regular and narrow (FIGURES 5-9). The distribution is symmetric and sometimes accentuated in the center of the lesion (FIGURES 10, 11).
In cutaneous malignant melanoma (CMM), the PN usually ends abruptly at the periphery and has irregular holes, thickened and darkened network lines, and tree-like branching at the periphery (FIGURES 12, 13). Moreover, in CMM the PN features change between different sectors of the PSL edge (border): some areas of malignant lesions manifest as a broad and prominent PN, while others have a discrete irregular PN; the PN may also be totally absent in some areas (FIGURES 12, 13).
Clinically atypical nevi (i.e., the nevi defined as dysplastic nevi at pathology evaluation) are often identified because they show areas of irregular and discrete PN distributed asymmetrically (FIGURES 14, 15).

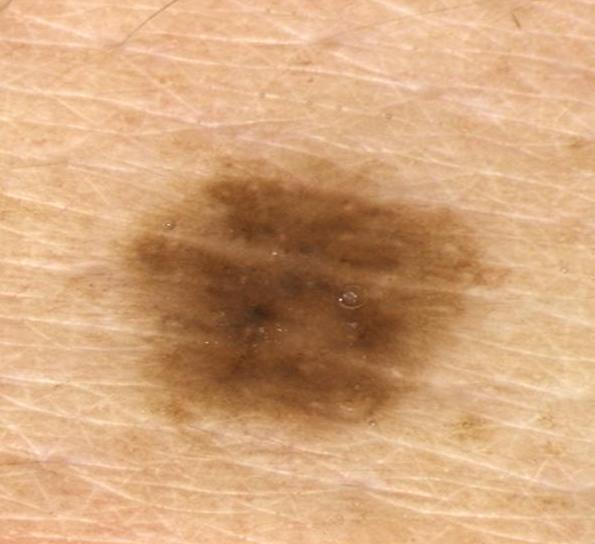

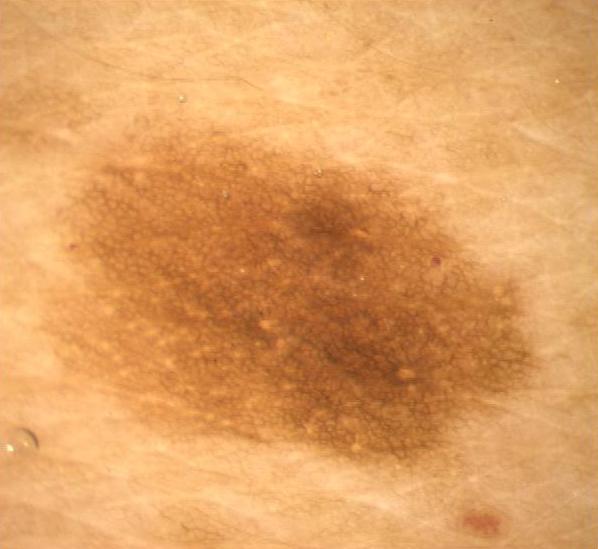





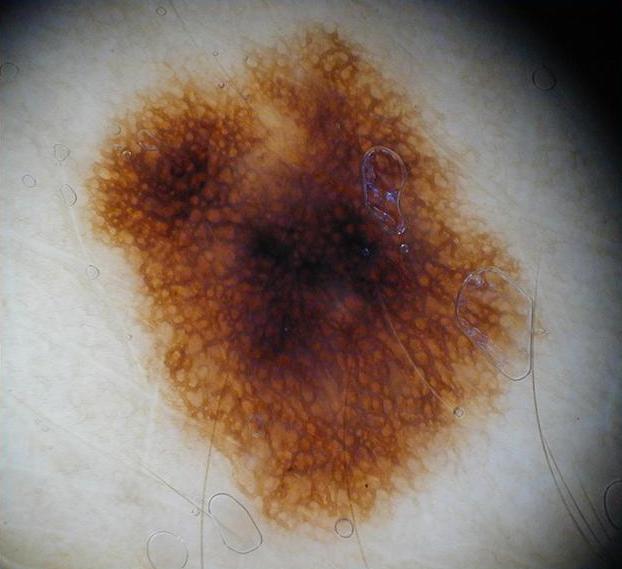

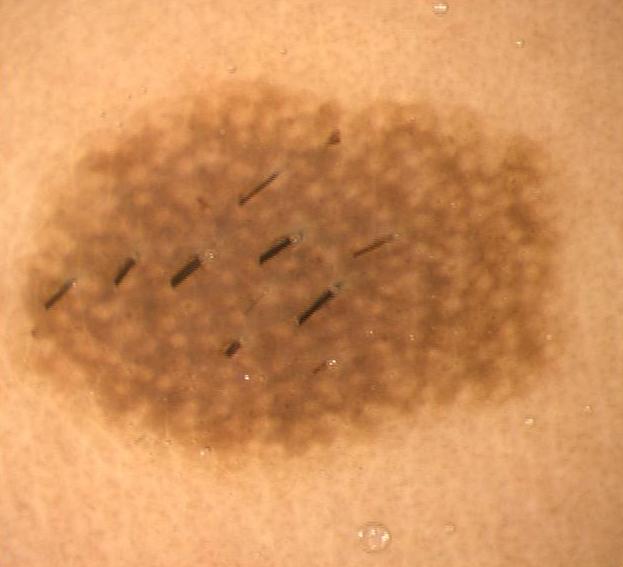



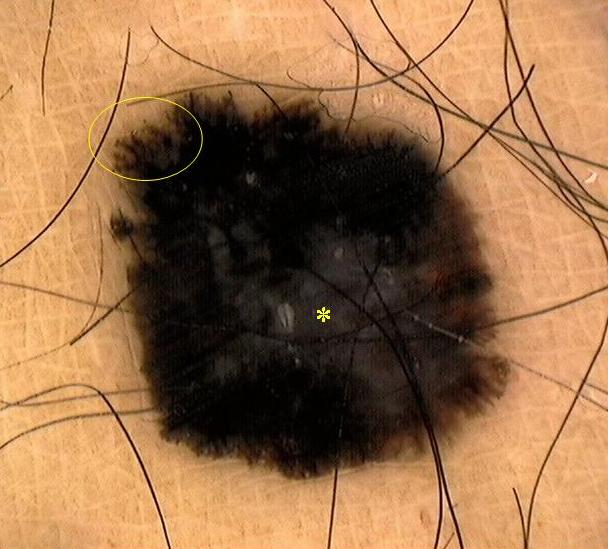



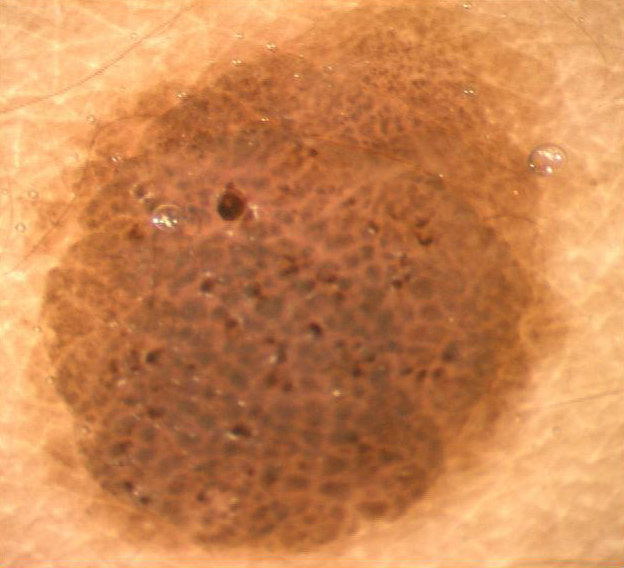
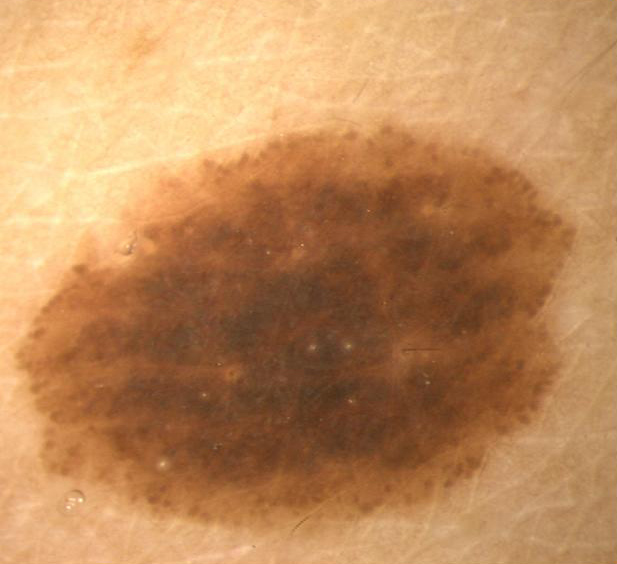
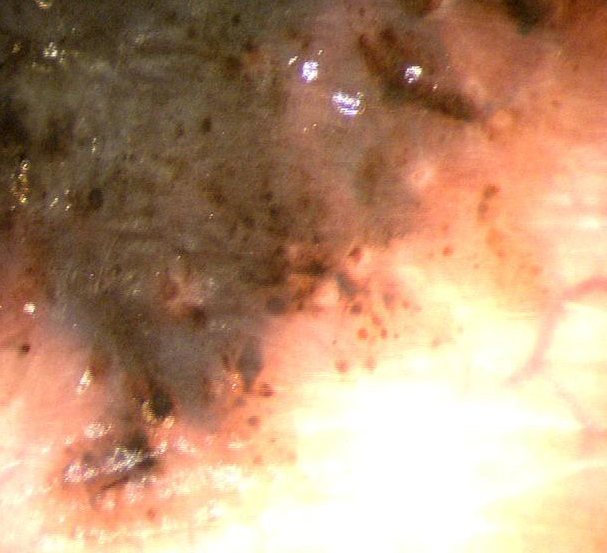

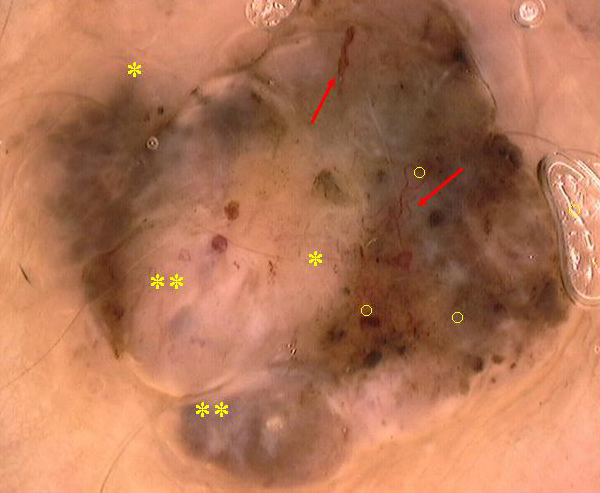
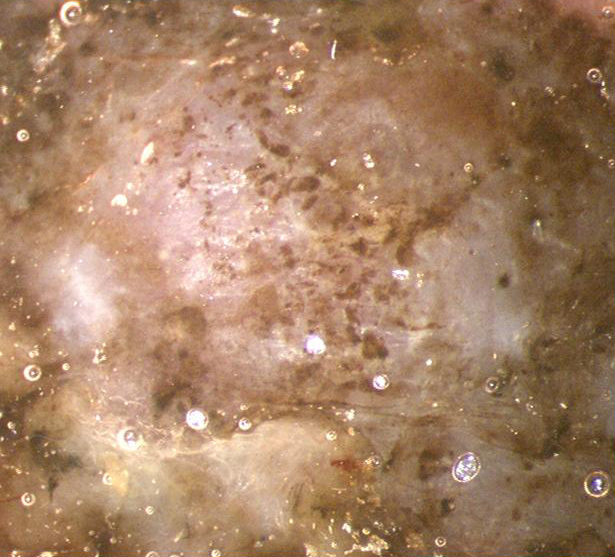

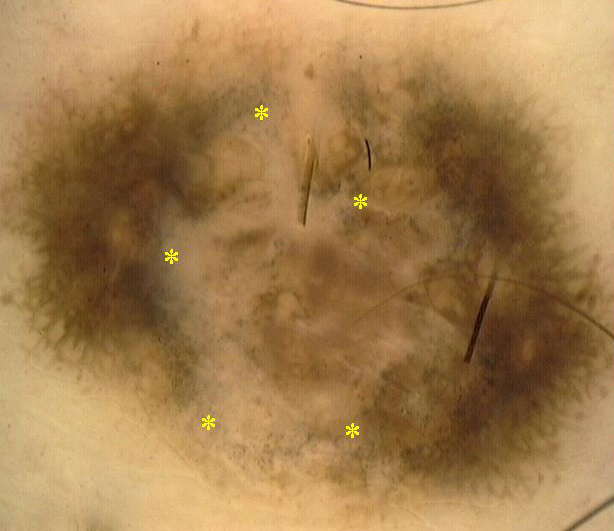


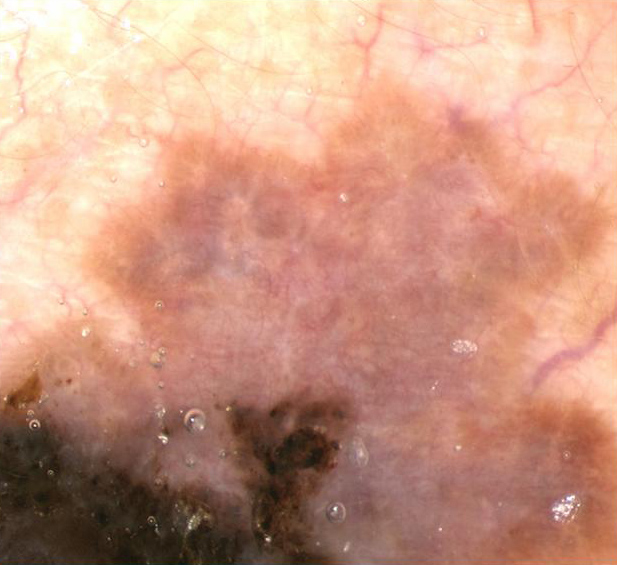
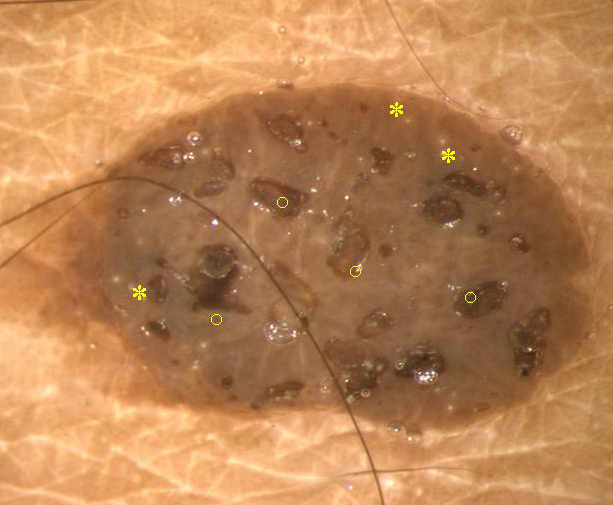





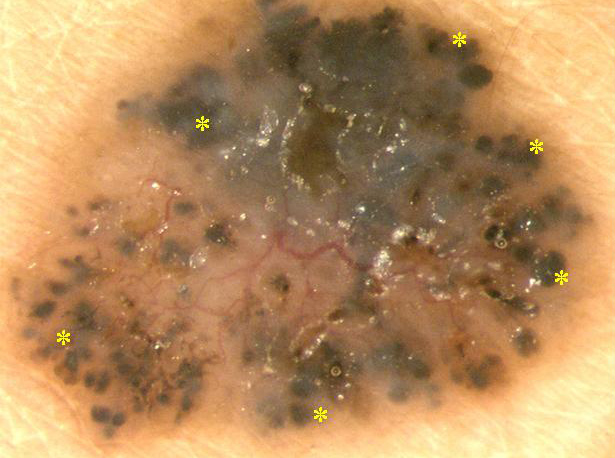




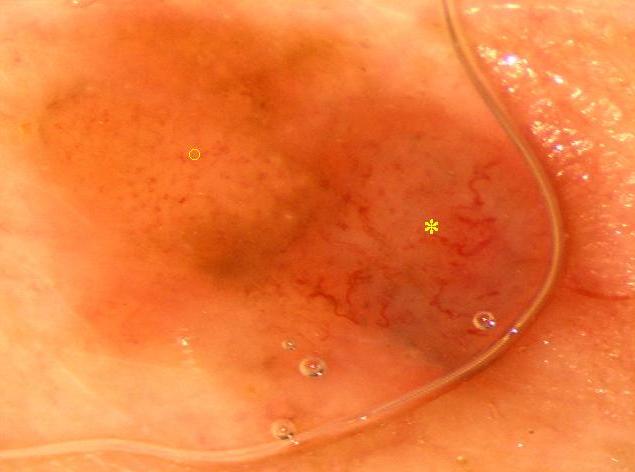
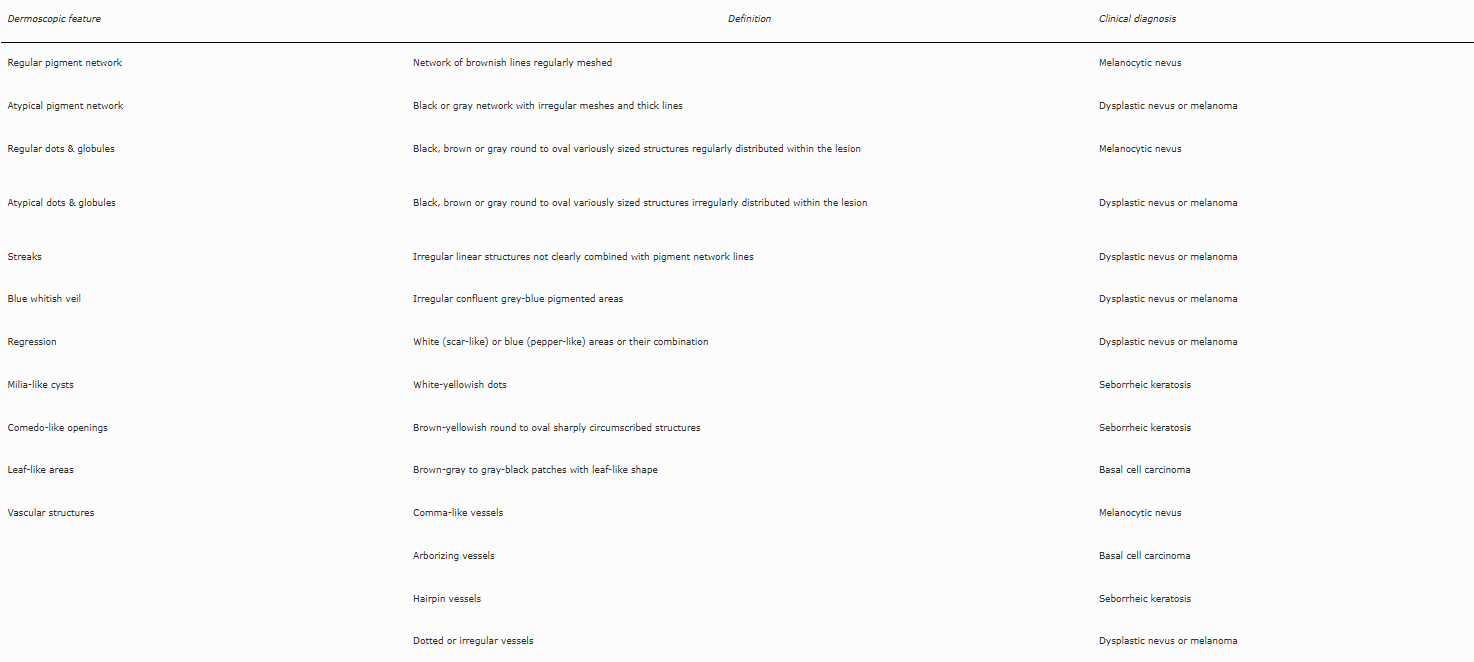
FIGURE 44: Pattern analysis.
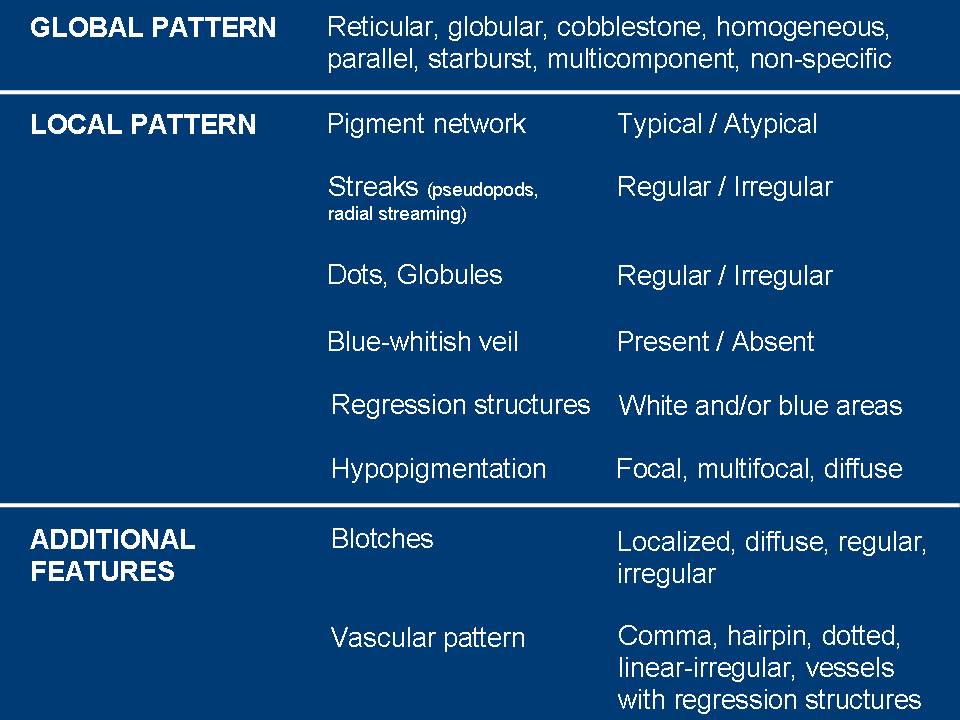

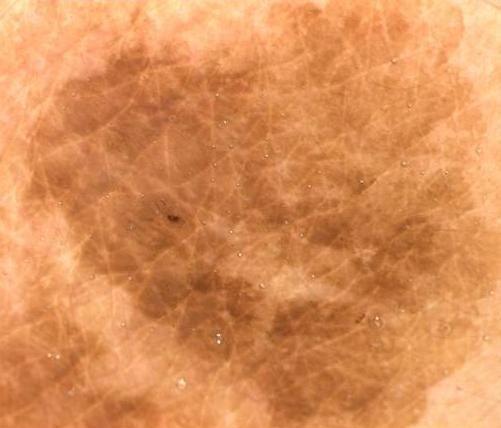
FIGURE 47: Pattern analysis: presence of one color, a regular design and a symmetrical pattern in benign nevi.




FIGURE 49: ABCD dermoscopy rule.
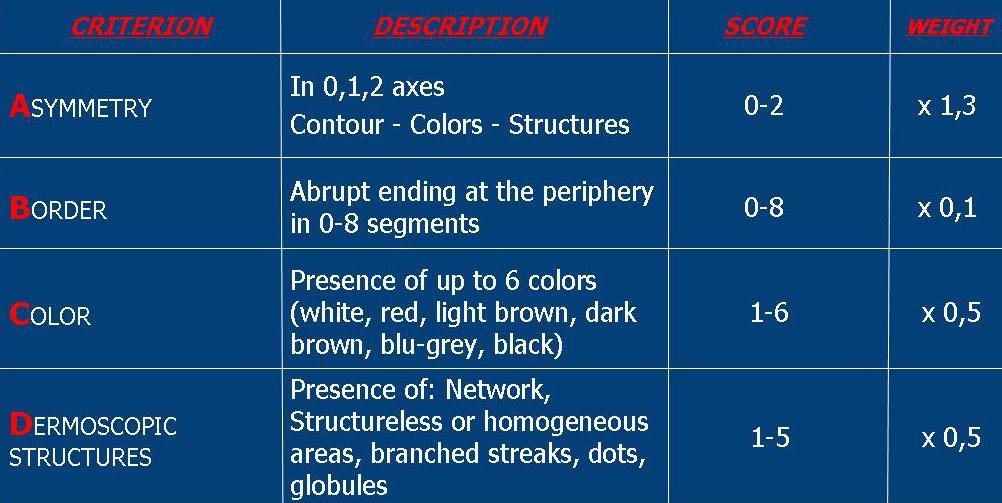
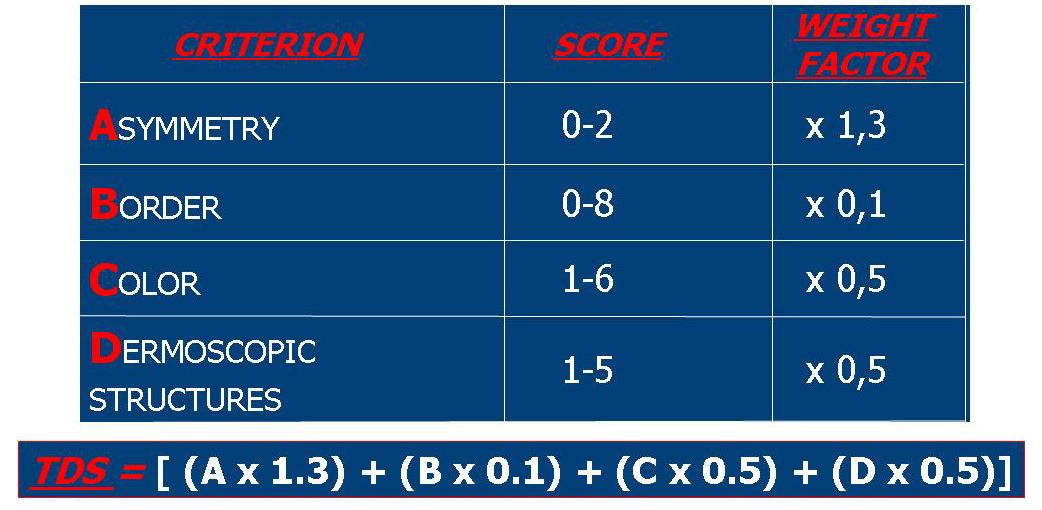
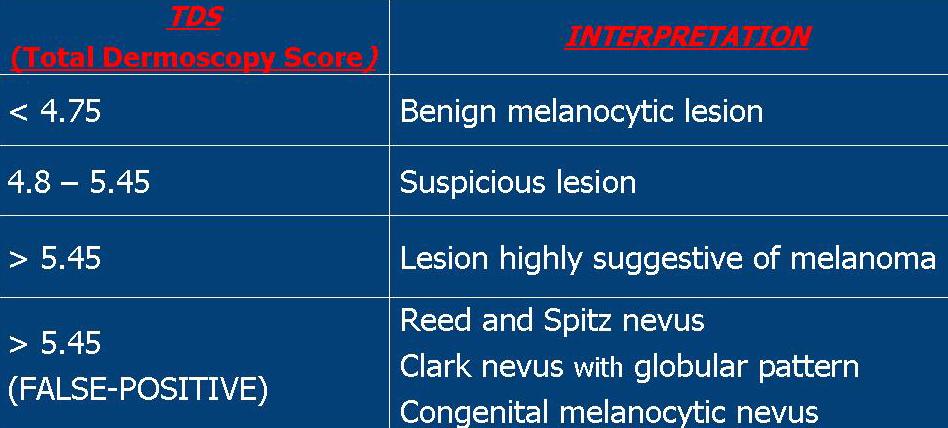
FIGURE 52: TDS examples: Clark nevus (upper panel) and cutaneous malignant melanoma (lower panel).
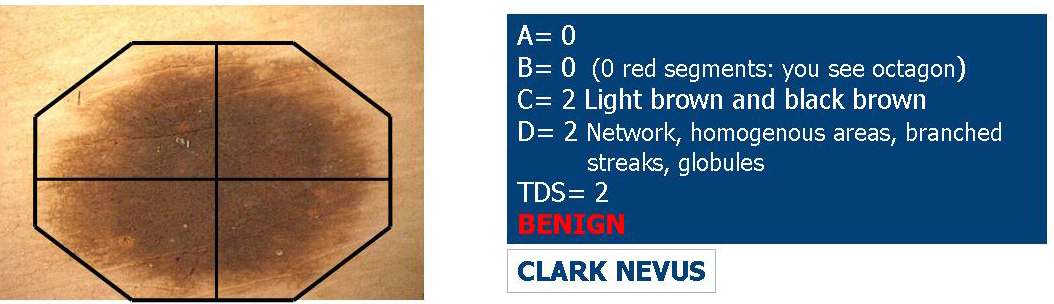
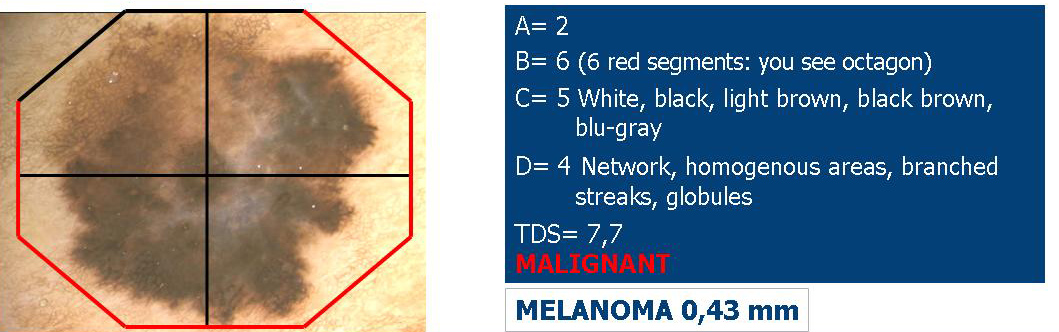
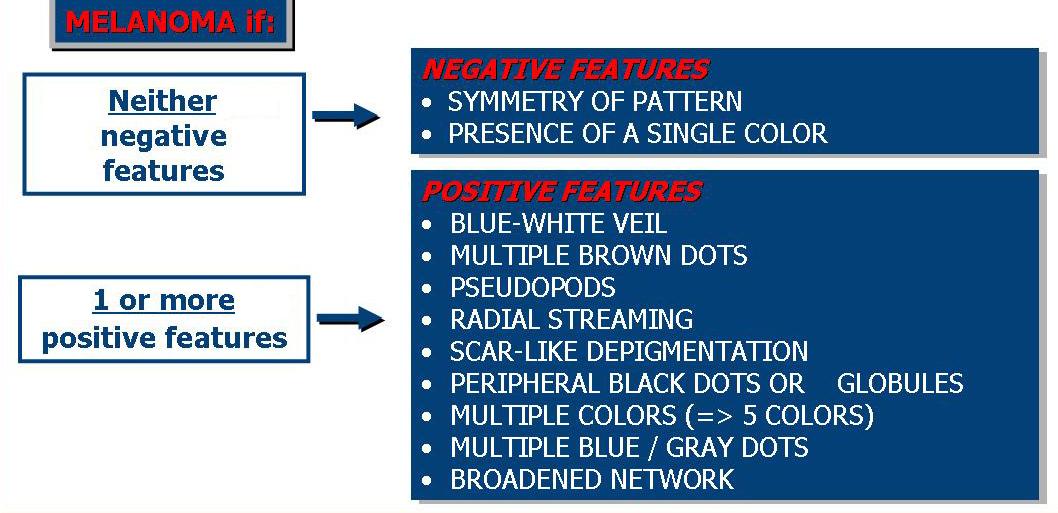
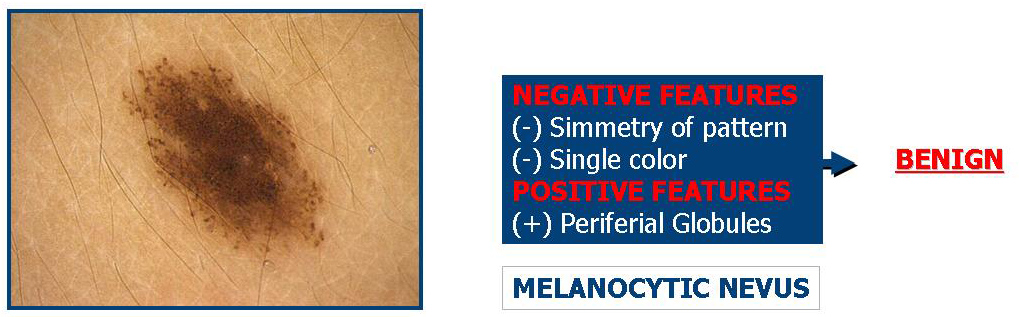
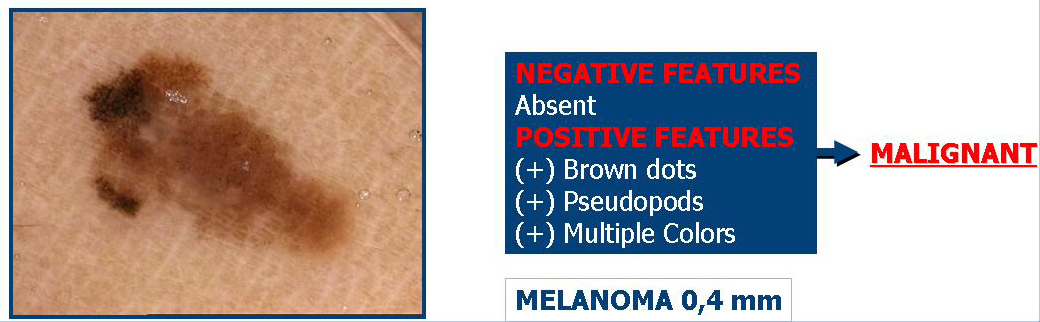
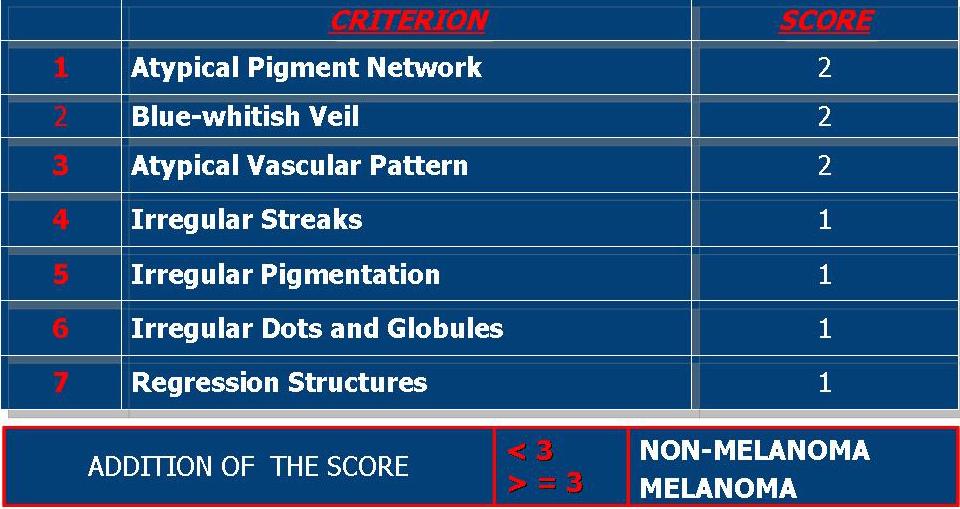
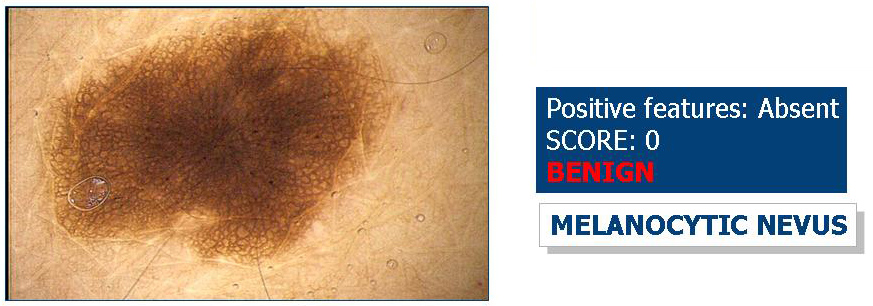
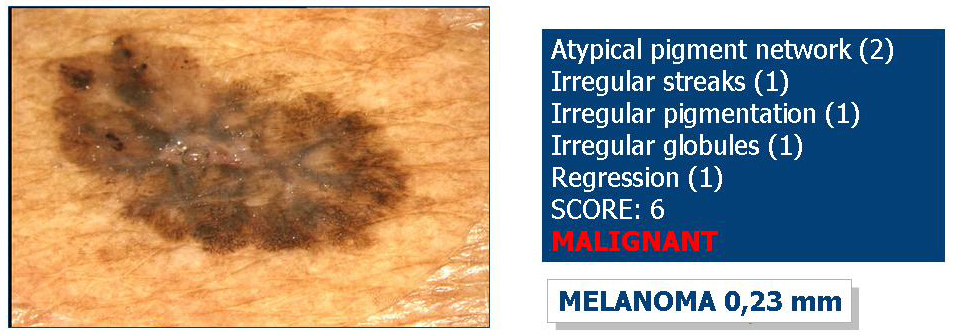
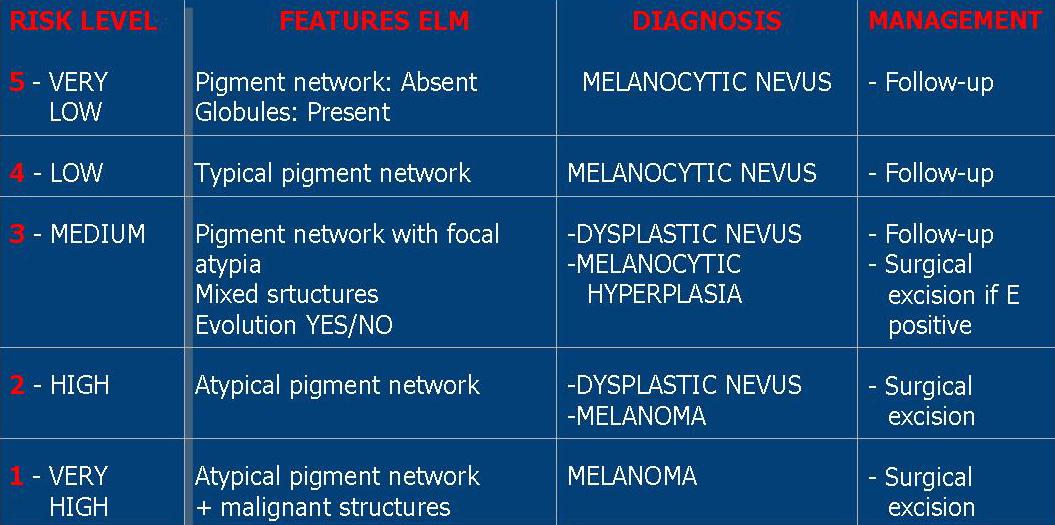
FIGURE 57: Risk level stratification.

The primary goal of melanoma detection is early tumor recognition and subsequent surgical treatment. The ABCD method for detecting cutaneous melanoma has been a useful tool in distinguishing benign lesions from melanoma. However, the clinical diagnosis of cutaneous melanoma may be difficult because some melanomas lack all or most of the features of the "ABCD" rule. In fact, some authors [29-31] have identified a subset of melanomas of unusual appearance, clinically indistinguishable from other pigmented and non-pigmented cutaneous lesions, that escape clinical recognition: the most common clinical diagnoses of these histopathologically confirmed melanomas were nevus, basal cell carcinoma, seborrheic keratosis, and lentigo, while the less common diagnoses included Bowen disease, verruca vulgaris, dermatofibroma, pyogenic granuloma, and hemangioma.
Dermoscopic diagnosis for melanoma also may be difficult because some cases lack specific features for melanoma. Some authors have demonstrated the limitations of dermoscopy in the detection of early melanomas that present with an uncharacteristic dermoscopic appearance. Some melanomas, the so-called "featureless melanomas," may lack specific dermoscopic features for melanoma diagnosis and dermoscopically may even appear as benign melanocytic lesions (nevus-like melanomas) or as atypical nevi, so that the diagnosis is impossible to make on dermoscopic grounds alone [22,30,31].
In fact, difficult melanomas present dermoscopic patterns indistinguishable from those of atypical nevi and common nevi. According some authors, melanomas that failed dermoscopic detection belong to the 3 following categories: melanomas showing criteria of melanocytic nevi, melanomas exhibiting criteria of non-melanocytic lesions, and melanomas lacking specific criteria of a melanocytic or non-melanocytic lesion (hypomelanotic/amelanotic melanoma) [22,30,31].
In addition, dermoscopy does not solve the dilemma of discriminating early, featureless melanoma from dysplastic nevi.
Only a meticulous comparative and interactive process based on an assessment of all the individual’s nevi ("ugly ducking" sign) and a knowledge about recent changes can lead to the recognition of melanomas that are difficult to diagnose [30].